Psilocybin's Dual Action: Rewiring Brain Circuits for Pain and Mood Relief
University of Pennsylvania researchers have discovered that psilocybin, the active compound in psychedelic mushrooms, can calm specific brain circuits associated with both pain and mood disorders. Their study reveals that psilocybin works in the anterior cingulate cortex, bypassing injury sites to provide dual relief for physical suffering and emotional distress. Unlike traditional opioids, this compound is non-addictive and may offer relief lasting up to two weeks, potentially revolutionizing chronic pain and depression treatment approaches.
Groundbreaking research from the University of Pennsylvania School of Medicine reveals that psilocybin, the active compound in psychedelic mushrooms, may offer a revolutionary approach to treating both chronic pain and mood disorders. This dual-action therapy targets specific brain circuits, providing hope for the millions worldwide who suffer from the interconnected challenges of physical pain and emotional distress.

Understanding Psilocybin's Mechanism
Psilocybin operates by gently activating serotonin receptors in the brain, specifically the 5-HT2A and 5-HT1A receptors. According to research published in Nature Neuroscience, this compound functions like a "dimmer switch" rather than fully turning brain signals on or off. This nuanced approach allows for precise modulation of brain activity without the harsh effects associated with traditional pain medications.
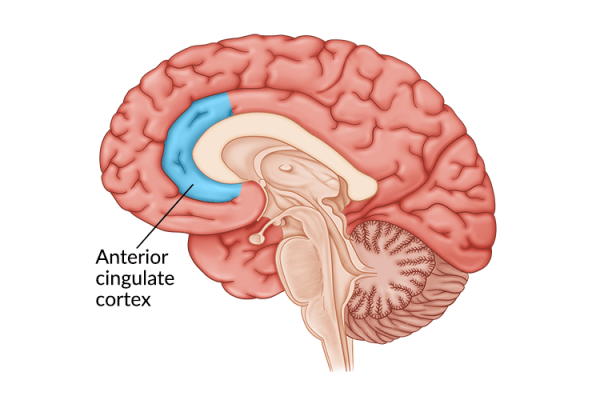
Targeting the Anterior Cingulate Cortex
The study identified the anterior cingulate cortex (ACC) as the primary site where psilocybin exerts its therapeutic effects. This brain region processes both pain signals and emotional responses, making it an ideal target for dual-action treatment. When researchers injected psilocin—the active metabolite of psilocybin—directly into the ACC, it provided the same pain relief and mood improvements as systemic administration.
Advantages Over Traditional Pain Management
Unlike opioid medications, which carry significant addiction risks and numerous side effects, psilocybin offers a non-addictive alternative. The research demonstrates that psilocybin bypasses injury sites entirely, instead modulating the brain circuits that process pain and emotional responses. This approach could fundamentally change how we treat chronic conditions that involve both physical and emotional components.
The study's findings are particularly significant given that chronic pain affects more than 1.5 billion people worldwide, often coexisting with depression and anxiety. This creates a vicious cycle where each condition amplifies the other, significantly impairing quality of life and making treatment more challenging.
Future Research Directions
While these findings are promising, researchers emphasize that more investigation is needed. The Penn team plans to study optimal dosing strategies, long-term effects, and the brain's ability to rewire itself to sustain therapeutic benefits. Understanding how multiple doses might adjust brain pathways involved in chronic pain could lead to longer-lasting solutions for patients.
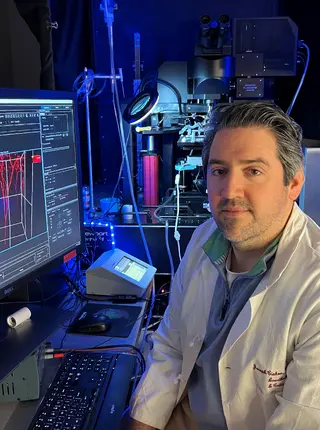
As Dr. Joseph Cichon, senior author of the study, notes, "These findings open the door to developing new, non-opioid, non-addictive therapies as psilocybin and related psychedelics are not considered addictive." The research was supported by funding from the National Institutes of Health and the American Society of Regional Anesthesia and Pain Medicine.
The discovery that psilocybin can provide relief from both pain and mood disorders through targeted brain circuit modulation represents a significant advancement in neuroscience and pain management. As research continues to evolve, this approach may offer new hope for patients seeking safer, more effective treatments for chronic conditions that have traditionally been difficult to manage.