How Fasting Enhances Breast Cancer Treatment: A New Scientific Discovery
A groundbreaking study published in Nature reveals the biological mechanism behind why periodic fasting can improve the effectiveness of endocrine therapy for breast cancer. Researchers have identified a specific hormone-signaling pathway and gene-expression changes in mice that explain this synergistic effect, offering new insights into overcoming treatment resistance. This discovery could pave the way for more effective, personalized treatment strategies for patients with hormone-receptor-positive breast cancer.
For patients with hormone-receptor-positive breast cancer, endocrine therapy is a cornerstone of treatment. However, the frequent development of resistance to drugs like tamoxifen presents a significant clinical hurdle. Emerging research suggests that dietary interventions, particularly periodic fasting, may hold a key to enhancing treatment efficacy. A landmark study published in Nature has now uncovered the precise biological mechanisms at play, offering a scientific explanation for this promising therapeutic synergy.

The Challenge of Treatment Resistance in Breast Cancer
The majority of breast cancers are characterized by the expression of the oestrogen receptor-α (ERα). Patients with this subtype are typically treated with endocrine therapy, which involves drugs that block oestrogen's effects, such as tamoxifen. Despite its effectiveness, a common and serious challenge is the eventual development of resistance to these therapies, leading to disease progression. This has driven the search for complementary strategies to boost treatment outcomes and delay resistance.
Fasting as a Potential Adjunct Therapy
Periodic fasting, conducted under strict clinical supervision, involves restricting calorie intake for specific periods on a regular cycle. Clinical observations have indicated that this practice can enhance the effectiveness of endocrine therapy. However, the underlying biological reasons for this effect have remained elusive, making it difficult to optimize and safely integrate into treatment protocols. Understanding the 'why' is crucial for translating anecdotal and preliminary clinical evidence into reliable medical practice.

The Discovery: Unraveling the Biological Mechanism
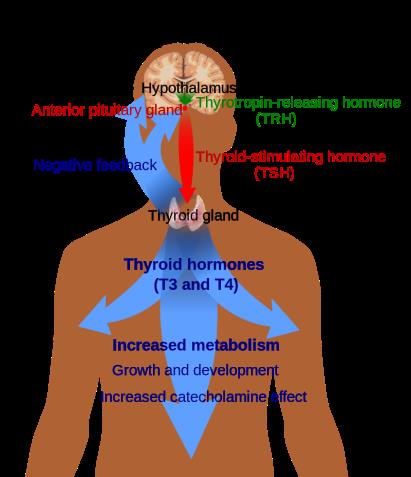
The new research by Padrão et al., published in Nature, provides critical answers. Conducted in mouse models, the study identified that fasting activates a specific hormone-signaling pathway involving glucocorticoids. This activation triggers a cascade of gene-expression changes within cancer cells. Essentially, fasting puts the body and the cancer cells in a metabolic state that makes them more susceptible to the anti-oestrogen effects of drugs like tamoxifen. This dual assault helps to overcome some of the cellular survival mechanisms that lead to treatment resistance.
Implications for Future Cancer Treatment
This discovery moves the conversation about fasting and cancer therapy from observation to mechanism. By pinpointing the glucocorticoid pathway and associated genetic changes, researchers now have a tangible target for further investigation. This opens several future avenues: developing drugs that mimic this fasting-induced pathway without requiring stringent dietary changes, creating biomarkers to identify patients who would benefit most from fasting protocols, and designing safer, more precise clinical fasting regimens tailored to enhance specific cancer treatments.
Conclusion and Cautious Optimism
The revelation of a clear biological link between fasting and improved breast cancer therapy efficacy is a significant step forward in oncology. It validates years of clinical interest and provides a scientific foundation for future research. However, it is crucial to emphasize that these findings are from preclinical mouse models. Fasting, especially for cancer patients, is a serious intervention that must only be undertaken under direct medical supervision. This research does not endorse unsupervised fasting but rather illuminates a promising path toward more effective, combination treatment strategies that could one day improve survival and quality of life for countless patients.