How Cannabis and Tobacco Co-Use Disrupts Brain Chemistry and Mood Regulation
Groundbreaking research from McGill University reveals that combining cannabis and tobacco creates distinct brain patterns that disrupt mood regulation. Scientists discovered elevated levels of an enzyme that breaks down anandamide, the brain's natural 'bliss molecule,' in co-users. This biochemical imbalance may explain why people who use both substances experience more anxiety, depression, and greater difficulty quitting cannabis. The findings represent the first human evidence of a molecular mechanism underlying the worsened outcomes observed in dual substance users.
New research from McGill University is shedding light on why people who use both cannabis and tobacco often experience more severe mood symptoms and greater difficulty quitting than those who use cannabis alone. The groundbreaking study reveals distinct brain chemistry patterns in co-users that disrupt the brain's natural mood regulation system, providing crucial insights into the complex interaction between these two commonly combined substances.

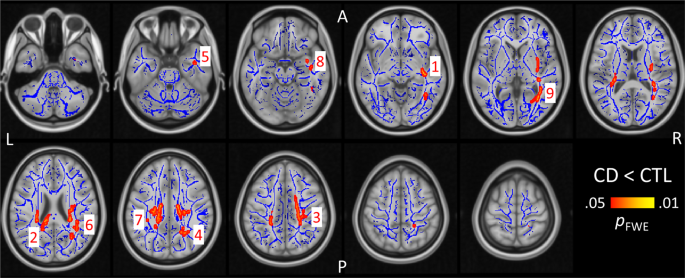
The Brain's Bliss Molecule Under Attack
The research team from McGill's Douglas Research Centre discovered that people using both cannabis and tobacco show elevated levels of an enzyme called FAAH (fatty acid amide hydrolase). This enzyme breaks down anandamide, a naturally occurring compound often described as the brain's "bliss molecule" due to its crucial role in regulating mood and stress responses. Higher FAAH levels directly translate to lower anandamide levels, creating a biochemical imbalance that has previously been linked to anxiety, depression, and higher relapse rates among people attempting to stop using cannabis.
According to lead author Rachel Rabin, Associate Professor in McGill's Department of Psychiatry, "This is the first evidence in humans of a molecular mechanism that may underlie why people who use both cannabis and tobacco experience worse outcomes." The findings, published in Drug and Alcohol Dependence Reports, represent a significant step forward in understanding the neurological basis of substance co-use complications.
Clinical Implications and Treatment Prospects
The discovery of this specific molecular mechanism opens new possibilities for developing targeted treatments for cannabis use disorder, particularly among individuals who also use tobacco. Currently, the only available treatments for cannabis dependence are behavioral therapies such as counseling. Identifying FAAH as a potential therapeutic target could lead to pharmacological interventions that address the underlying brain chemistry disruptions.
As Professor Rabin explained, "Identifying this mechanism is an important step toward finding targets for future medications to treat cannabis use disorder, especially among those that co-use tobacco." The research team's findings suggest that addressing the FAAH-anandamide imbalance could potentially improve treatment outcomes for dual substance users who have historically faced greater challenges in achieving sustained recovery.
Research Methodology and Future Directions
The preliminary investigation involved 13 young adults, with eight participants using only cannabis and five using both cannabis and cigarettes daily. Cannabis consumption averaged slightly above one gram per day, while cigarette use ranged from one to twelve cigarettes daily. The researchers used PET scans to measure brain activity and enzyme levels, revealing striking differences between the two groups.
Co-author Romina Mizrahi, Professor of Psychiatry and director of the McGill Research Center for Cannabis, noted the unexpected strength of the findings: "What surprised us was how strong the effect was, and how different it was from those who only used cannabis, compared to those who used both tobacco and cannabis." The research team is now expanding their investigation to include people who smoke cigarettes and vape nicotine without cannabis use to determine whether similar brain changes occur with tobacco alone.

Public Health Significance
This research addresses a critical gap in substance use literature, as most previous studies have focused on cannabis and tobacco separately despite their frequent co-use. In Canada, while overall tobacco use is declining, the majority of cannabis users still report using tobacco alongside cannabis. Approximately one in twenty people who used cannabis within the past year are considered at risk for cannabis use disorder, with this rate jumping to about one in three among frequent cannabis users.
The study's findings have significant implications for public health approaches to substance use treatment and prevention. Understanding the specific neurological mechanisms that make co-use particularly challenging could lead to more effective intervention strategies and better support for individuals struggling with multiple substance dependencies.
The research received funding from the National Institute of Mental Health and represents an important contribution to the growing body of evidence about how different substances interact within the brain's complex chemistry. As legal cannabis use becomes more widespread in many regions, understanding these interactions becomes increasingly crucial for developing effective public health policies and treatment protocols.