MIT and Harvard Develop 'Stealth' Immune Cells for Off-the-Shelf Cancer Treatment
Scientists from MIT and Harvard Medical School have engineered advanced CAR-NK immune cells that can effectively destroy cancer while evading the body's immune defenses. This breakthrough enables the creation of 'off-the-shelf' cancer therapies that could be available immediately after diagnosis, eliminating the weeks-long wait required for personalized cell treatments. The innovation addresses one of the major limitations in current cancer immunotherapy by preventing immune rejection of donor cells.
Cancer treatment may be on the verge of a revolutionary transformation as researchers from MIT and Harvard Medical School have developed engineered immune cells that can effectively target cancer while remaining undetected by the body's own immune defenses. This breakthrough in cellular immunotherapy could dramatically change how cancer patients receive treatment, potentially making powerful therapies available within days rather than weeks of diagnosis.
The Challenge with Current Cell Therapies
Traditional cancer immunotherapies like CAR-T cells have shown remarkable success in treating certain blood cancers, but they come with significant limitations. The current approach requires extracting a patient's own immune cells, genetically engineering them to target cancer, and then growing enough cells for treatment—a process that typically takes several weeks. For patients with aggressive cancers, this delay can be critical. Additionally, using donor cells from healthy individuals has been problematic because the recipient's immune system often recognizes these cells as foreign and destroys them before they can attack the cancer.
Engineering Stealth CAR-NK Cells
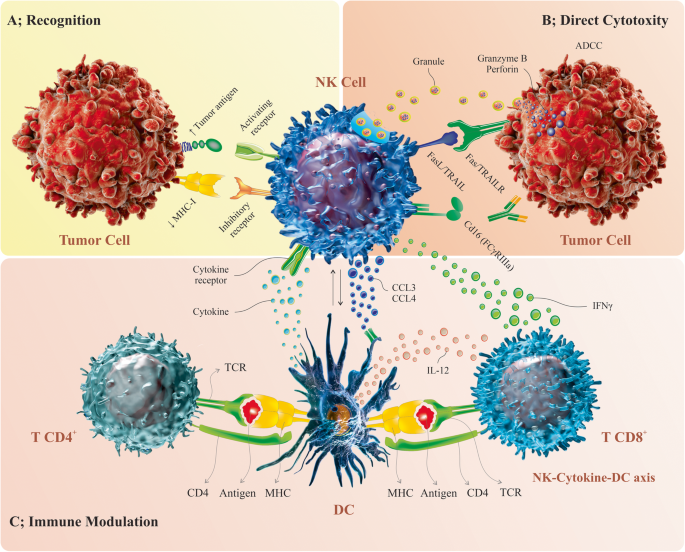
The MIT and Harvard team focused on natural killer (NK) cells, which are part of the body's innate immune system and naturally target abnormal or infected cells. By engineering these cells to express chimeric antigen receptors (CARs), researchers created CAR-NK cells programmed to recognize specific cancer markers. The key innovation lies in making these cells 'stealth' by removing surface proteins called HLA class 1 molecules that normally act as identity markers for the immune system.
How the Technology Works
The researchers developed a single DNA construct that incorporates multiple genetic modifications. This construct includes siRNA to silence genes producing HLA class 1 proteins, the CAR gene for cancer targeting, and additional genes encoding PD-L1 or single-chain HLA-E to enhance the cells' cancer-fighting capabilities. This comprehensive approach allows for efficient conversion of donor NK cells into immune-evasive CAR-NK cells that can target specific cancer proteins like CD-19, commonly found on malignant B cells in lymphoma patients.
Proven Effectiveness in Preclinical Models
In tests using mice with humanized immune systems, the newly engineered CAR-NK cells demonstrated remarkable effectiveness. Mice receiving the stealth CAR-NK cells maintained the therapeutic cell population for at least three weeks, and the cells nearly eliminated cancer in these subjects. In contrast, mice receiving either unmodified NK cells or NK cells with only the CAR gene saw their donor cells attacked and eliminated by the host immune system within two weeks, allowing cancer to spread unchecked.

Safety Advantages and Future Applications
Beyond their effectiveness against cancer, the engineered CAR-NK cells showed a significantly reduced likelihood of causing cytokine release syndrome—a common and potentially life-threatening side effect of current immunotherapy treatments. This improved safety profile suggests that CAR-NK cells could eventually replace CAR-T cells in many applications. The researchers are now planning clinical trials through Dana-Farber Cancer Institute and are also exploring applications beyond cancer, including using CAR-NK cells to treat autoimmune disorders like lupus.
Transforming Cancer Treatment Accessibility
The ability to create off-the-shelf CAR-NK treatments represents a major advancement in making advanced cancer therapies more accessible. Rather than waiting weeks for personalized cell manufacturing, hospitals could maintain supplies of pre-engineered CAR-NK cells ready for immediate use after diagnosis. This approach could be particularly valuable for patients whose own cells may not be healthy enough for reliable use in traditional cell therapy manufacturing processes.
The development of stealth CAR-NK cells marks a significant step forward in cancer immunotherapy, addressing key limitations of current treatments while opening new possibilities for rapid, effective cancer care. As this technology moves toward clinical trials, it holds the potential to transform how we approach cancer treatment, making powerful cellular therapies more accessible and effective for patients worldwide.





