Restoring Brain Blood Flow: A New Frontier in Dementia Treatment
A groundbreaking study from the University of Vermont reveals that dementia may be driven by faulty blood flow in the brain caused by the loss of a key lipid molecule called PIP2. Researchers discovered that when PIP2 levels drop, the pressure-sensing protein Piezo1 becomes overactive, disrupting cerebral circulation and starving brain tissue. Remarkably, restoring this missing molecule normalized blood flow in preclinical models, pointing to a promising new therapeutic approach for vascular problems in dementia. This research offers hope for millions affected by Alzheimer's and related disorders.
Dementia represents one of the most significant global health challenges of our time, affecting millions of families and straining healthcare systems worldwide. While research has traditionally focused on protein plaques, inflammation, and neural degeneration, a groundbreaking study from the University of Vermont has uncovered a potentially crucial vascular component. Published in the Proceedings of the National Academy of Sciences, this research reveals how faulty blood flow in the brain, driven by the loss of a specific lipid molecule, may contribute to dementia progression—and how restoring this molecule could open new treatment pathways.
.jpg?sfvrsn=e59f647a_0&MaxWidth=600&MaxHeight=325&ScaleUp=false&Quality=High&Method=ResizeFitToAreaArguments&Signature=0F24AEFED6347CB2AE39DD073316E2064A9B4CBC)
The study centers on cerebral blood flow regulation, a critical process for delivering oxygen and nutrients to brain tissue. When this circulation falters, brain cells become starved and vulnerable to damage, potentially accelerating cognitive decline. The University of Vermont team, led by principal investigator Dr. Osama Harraz, has identified a precise molecular mechanism behind this vascular dysfunction, offering what Dr. Harraz describes as "a huge step forward in our efforts to prevent dementia and neurovascular diseases."
The Piezo1 Protein and Blood Flow Regulation
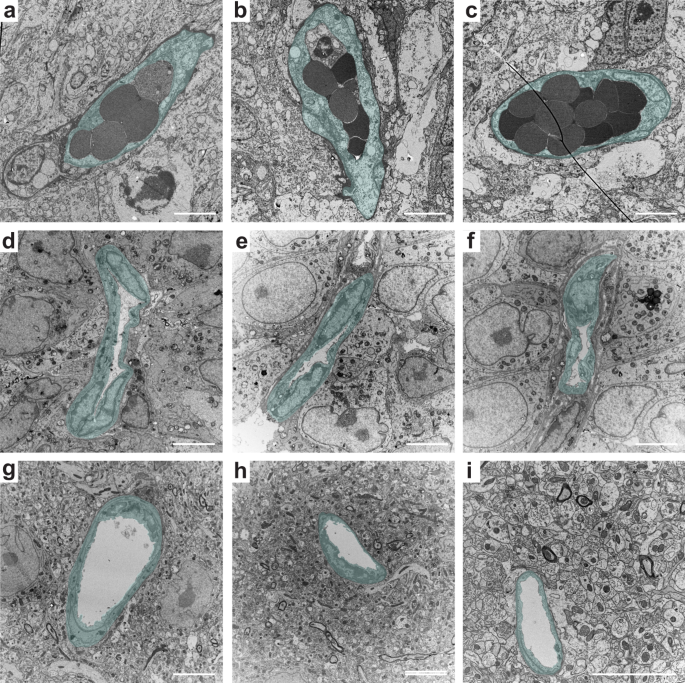
At the heart of this discovery is a protein called Piezo1, named from the Greek word for "pressure." Found in the membranes of cells lining blood vessels, Piezo1 acts as a mechanical sensor, detecting physical forces created as blood moves through the brain's intricate vascular network. This protein helps regulate cerebral blood flow by responding to pressure changes, essentially telling blood vessels when to constrict or dilate to maintain optimal circulation.
Previous research had shown that Piezo1 behaves differently in people with certain genetic variations, suggesting its importance in vascular health. The new study builds on this foundation by examining what happens when Piezo1 regulation goes awry. Researchers discovered that in conditions like Alzheimer's disease, Piezo1 becomes abnormally overactive in brain blood vessels, leading to disrupted circulation patterns that deprive brain tissue of essential resources.

The Missing Molecule: PIP2 as a Natural Suppressor
The breakthrough came when researchers investigated why Piezo1 becomes overactive in dementia. They focused on a phospholipid called PIP2 (phosphatidylinositol 4,5-bisphosphate), which is naturally present in brain cell membranes and plays essential roles in cell signaling and ion channel regulation. Ion channels like Piezo1 are protein pores that control the flow of ions in and out of cells, a process fundamental to cellular communication and function.
The research team discovered that PIP2 normally acts as a natural suppressor of Piezo1 activity. When PIP2 levels are adequate, it keeps Piezo1 in check, preventing excessive channel opening and maintaining normal blood flow. However, in dementia-related conditions, PIP2 levels decline significantly. Without this regulatory control, Piezo1 channels remain persistently overactive, disrupting the delicate balance of cerebral blood circulation.
Restoring Normal Function
The most promising aspect of this research emerged when scientists tested whether restoring PIP2 could reverse the vascular dysfunction. In preclinical models, when the research team added PIP2 back into the system, Piezo1 activity decreased appropriately, and healthy blood circulation was restored. This finding suggests that increasing PIP2 levels could form the basis of a new treatment strategy aimed at improving brain blood flow and supporting cognitive function in dementia patients.
The study, titled "PIP2 Corrects an Endothelial Piezo1 Channelopathy," provides compelling evidence that vascular problems in dementia might be treatable by addressing this specific molecular imbalance. As Dr. Harraz explains, "We are uncovering the complex mechanisms of these devastating conditions, and now we can begin to think about how to translate this biology into therapies."
Future Directions and Therapeutic Potential
While this research represents a significant advance, several important questions remain. Future studies will focus on understanding exactly how PIP2 interacts with Piezo1 at the molecular level. Researchers want to determine whether PIP2 attaches directly to specific parts of the Piezo1 protein or changes the surrounding cell membrane in ways that limit channel opening. Additional work will explore how disease-related declines in PIP2 occur and whether other factors contribute to removing this regulatory control.
Gaining clarity on these mechanisms will be critical for developing targeted therapies. Potential approaches could include developing drugs that restore PIP2 levels, creating compounds that mimic PIP2's suppressive effects on Piezo1, or designing treatments that directly modulate Piezo1 activity to improve neurovascular health. The research also opens possibilities for early intervention strategies that might prevent vascular dysfunction before significant cognitive decline occurs.
Broader Implications for Dementia Treatment
This discovery adds an important dimension to our understanding of dementia, which affects approximately 50 million people worldwide with numbers continuing to grow. Traditional approaches have focused primarily on protein accumulation (like amyloid-beta and tau in Alzheimer's disease) and inflammation. The vascular component highlighted in this research suggests that comprehensive dementia treatment might require addressing multiple interconnected systems—neural, inflammatory, and now vascular.
The finding that restoring a single molecule can normalize blood flow in preclinical models offers hope for developing more effective interventions. It also underscores the importance of continued investment in basic scientific research that uncovers fundamental biological mechanisms. As the global burden of dementia increases, placing heavy pressure on families, caregivers, and healthcare systems, such discoveries provide crucial stepping stones toward better treatments and prevention strategies.
In conclusion, the University of Vermont research represents a significant advance in our understanding of dementia's vascular components. By identifying PIP2 as a key regulator of cerebral blood flow through its suppression of Piezo1 activity, and demonstrating that restoring this molecule can normalize circulation, scientists have opened a promising new avenue for therapeutic development. While much work remains to translate these findings into clinical treatments, this research offers genuine hope that targeting vascular dysfunction could become an important part of comprehensive dementia care in the future.





