Historic Pediatric Dual Organ Transplant: A Milestone in Children's Healthcare
Children's Hospital Colorado has achieved a historic medical milestone by successfully completing its first-ever pediatric dual heart and liver transplant. The life-saving 16-hour surgery was performed on 11-year-old Gracie Greenlaw, who was born with a complex congenital heart condition that led to liver failure. This article explores the groundbreaking procedure, the years of multidisciplinary preparation by dozens of specialists, and what this achievement means for the future of pediatric transplant care.
In a landmark achievement for pediatric medicine, Children's Hospital Colorado has successfully performed its first-ever dual heart and liver transplant on a child, marking a significant advancement in complex organ transplantation. This historic procedure, completed on 11-year-old Gracie Greenlaw, represents not just a surgical triumph but the culmination of years of meticulous preparation by dozens of specialized medical professionals. The successful outcome demonstrates how coordinated, multidisciplinary care can overcome even the most challenging medical scenarios, offering new hope for children with life-threatening organ conditions.

The Groundbreaking Procedure
The dual organ transplant at Children's Hospital Colorado represents a rare and complex medical achievement. According to the hospital's announcement, only 38 pediatric patients nationwide had previously received both a heart and liver transplant before Gracie's procedure. The surgery required precise coordination between multiple surgical teams working simultaneously on different organ systems, with the entire operation spanning 16 hours of continuous medical attention.
Dr. Megan Adams, surgical director of the Pediatric Liver Transplant and Kidney Transplant Programs at Children's Colorado, emphasized the significance of this achievement: "Performing Children's Colorado's first-ever heart and liver dual organ transplant is an amazing accomplishment for our Pediatric Transplant Program. Thanks to years of dedication and a team committed to being the trusted leaders in pediatric transplant across our seven-state region, we're grateful to provide this level of care to even more kids who need complex organ transplants."

Patient Background and Medical Journey
Gracie Greenlaw's medical journey began at birth with a diagnosis of hypoplastic left heart syndrome (HLHS), a congenital condition where the heart develops with only one functioning pumping chamber. Before turning three years old, she underwent three major cardiac surgeries—the Norwood, Glenn, and Fontan procedures—to help her heart circulate blood effectively. While these surgeries allowed her to survive, they created long-term complications that eventually led to liver damage and failure.
Dr. Kathleen Simpson, a cardiologist involved in Gracie's care, explained the progression: "The Fontan is a lifesaving surgery, but the longer someone lives after the procedure, there is an increased chance of developing comorbidities. Our care team worked to keep her healthy and living a typical day-to-day life as long as possible before we determined a dual organ transplant would give her the best long-term quality of life." Gracie's condition worsened over the past year with the development of plastic bronchitis and signs of liver failure, ultimately necessitating the dual transplant approach.
Years of Preparation and Multidisciplinary Coordination
The success of this historic transplant didn't happen overnight. Care teams at Children's Colorado had spent years preparing for the possibility of a dual heart and liver transplant. This preparation involved close coordination among specialists in surgery, cardiology, hepatology, and numerous other fields, supported by strong hospital leadership commitment to advancing transplant capabilities.
A key component of this preparation was the establishment of the Fontan Multidisciplinary Clinic in 2016 as part of the hospital's Single Ventricle Program. This clinic specifically focuses on caring for patients with HLHS and other single ventricle conditions by providing coordinated, whole-patient care. Through this program, Gracie received continuous monitoring and treatment from a team that included both cardiologists like Dr. Simpson and hepatologists like Dr. Dania Brigham, ensuring comprehensive management of both her heart and liver conditions until transplantation became necessary.

The Surgical Procedure and Technological Innovation
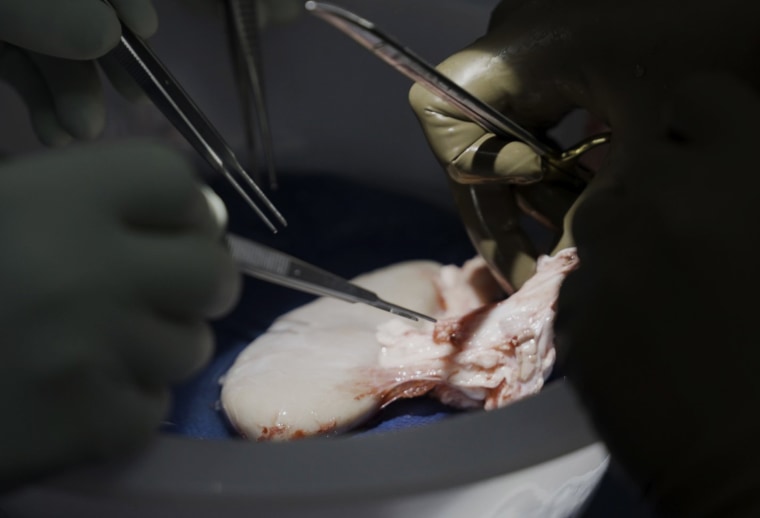
The actual transplant surgery represented a marvel of medical coordination and technological innovation. When compatible donor organs became available less than a month after Gracie joined the transplant waitlist, the surgical team sprang into action. Because the heart can only remain viable for a short time outside the body, the team began with the heart transplant, led by Dr. Matthew Stone, surgical director of the Pediatric Heart Transplant Program, and congenital heart surgeon Dr. Emily Downs in a nine-hour procedure.
Meanwhile, the donor liver was maintained on a TransMedics Organ Care System—a specialized device designed to replicate normal liver function. This technology preserved the liver and allowed the heart surgeons the time they needed to complete their work before Dr. Adams and transplant surgeon Dr. Kendra Conzen performed the seven-hour liver transplant. Throughout the entire process, close coordination with anesthesiology teams was essential to protect Gracie's health during this physically demanding procedure.
Recovery and Future Outlook
The surgery proved successful, with Gracie leaving the cardiac progress care unit just over a month later. Seven months post-transplant, she continues to attend monthly follow-up visits but has returned to school and normal life at home with her family and dogs. While she will need another heart transplant later in life—as is typical for pediatric heart transplant recipients—her transplanted liver is expected to last for her lifetime.
Dr. Duncan Wilcox, Surgeon in Chief at Children's Hospital Colorado, highlighted the broader implications of this achievement: "This procedure showcases the expertise, talent and level of care Children's Colorado provides to our patients, including those with complex medical needs. As the top-ranked pediatric hospital in Colorado and the Rocky Mountain region, we are proud of our leading-edge transplant care and look forward to supporting more patients who need dual organ transplants in the future." This historic transplant not only saved one child's life but established new capabilities that will benefit countless other children facing similar medical challenges.