Weight-Loss Surgery Outperforms GLP-1 Medications for Long-Term Health Benefits
A comprehensive Cleveland Clinic study reveals that weight-loss surgery provides superior long-term health outcomes compared to GLP-1 medications for patients with obesity and diabetes. Over a 10-year period, surgical patients experienced significantly lower risks of death, heart disease, kidney failure, and eye complications. The research demonstrates that metabolic surgery offers unique survival advantages and better weight maintenance, even as powerful new obesity drugs become available. These findings highlight the continued importance of surgical interventions in comprehensive diabetes and obesity management.
New research from Cleveland Clinic provides compelling evidence that weight-loss surgery delivers superior long-term health outcomes compared to GLP-1 receptor agonist medications for individuals living with both obesity and type 2 diabetes. The landmark study, published in Nature Medicine, followed nearly 4,000 patients over a decade, revealing that surgical intervention offers significant advantages in longevity and complication reduction that medication alone cannot match.

Comparative Health Outcomes
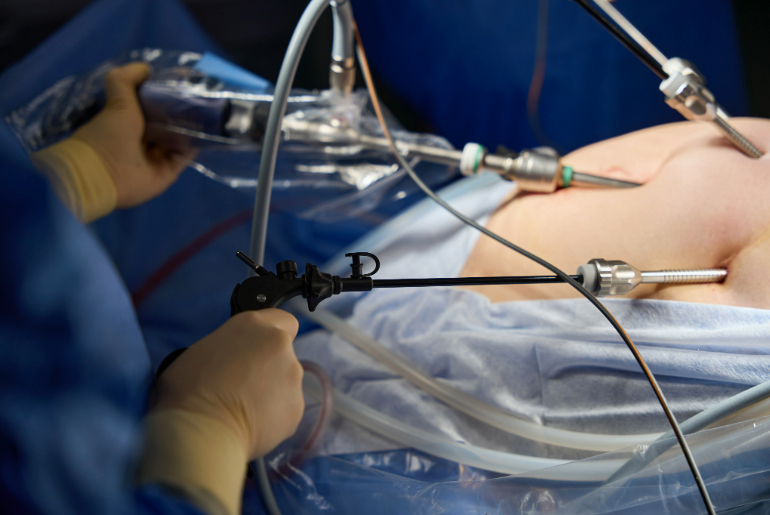
The M6 study (Macrovascular and Microvascular Morbidity and Mortality after Metabolic Surgery versus Medicines) tracked 3,932 adults with obesity and diabetes receiving care at Cleveland Clinic. Participants were divided into two groups: 1,657 who underwent metabolic surgery procedures such as gastric bypass or sleeve gastrectomy, and 2,275 who were treated with GLP-1 medications including semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), dulaglutide (Trulicity), exenatide (Byetta, Bydureon), and tirzepatide (Mounjaro, Zepbound).
Significant Risk Reduction Benefits
After 10 years of follow-up, the surgical group demonstrated dramatically better health outcomes across multiple critical metrics. Patients who underwent weight-loss surgery experienced a 32% lower risk of death compared to those using GLP-1 medications alone. The cardiovascular benefits were equally impressive, with surgical patients showing a 35% reduction in major heart problems including heart attack, heart failure, and stroke.
Organ Protection Advantages
The protective effects extended to vital organs, with surgical patients experiencing a 47% lower risk of serious kidney disease and a remarkable 54% reduction in diabetes-related eye damage (retinopathy). These microvascular complications represent some of the most debilitating consequences of long-term diabetes, and the substantial risk reduction highlights the profound impact of surgical intervention on disease progression.
Weight Loss and Metabolic Control
The comparative effectiveness extended to weight management and metabolic control. Surgical patients lost an average of 21.6% of their body weight, significantly outperforming the 6.8% weight loss achieved by medication users. Blood sugar control, measured by hemoglobin A1c levels, also improved more substantially with surgery (-0.86%) compared to medication (-0.23%). This superior metabolic control translated into practical benefits, with surgical patients requiring fewer prescriptions for diabetes, blood pressure, and cholesterol management over the long term.

Clinical Implications and Future Directions
According to Dr. Ali Aminian, director of Cleveland Clinic's Bariatric & Metabolic Institute and primary investigator of the study, "Even with today's best medicines, metabolic surgery offers unique and lasting benefits for people with obesity and diabetes. The benefits we observed went beyond weight loss." Dr. Steven Nissen, Chief Academic Officer of the Heart, Vascular & Thoracic Institute at Cleveland Clinic and senior author, emphasized that "Even in the era of these powerful new drugs to treat obesity and diabetes, metabolic surgery may provide additional benefits, including a survival advantage."
The researchers note that while the study has limitations—being observational rather than randomized and not focusing exclusively on the newest GLP-1 medications—the findings strongly support maintaining surgical options as part of comprehensive obesity and diabetes management. Future research should directly compare surgery with the latest GLP-1 therapies to further refine treatment guidelines and help healthcare providers and patients make informed decisions about the most appropriate interventions for long-term health.




