Liver mRNA Therapy Rejuvenates Aged Immune Systems in Mice
A groundbreaking study published in Nature demonstrates how mRNA therapy can reverse age-related immune decline. Researchers successfully used lipid nanoparticles to deliver three immune-stimulating mRNAs to the liver of aged mice, effectively restoring T cell function, thymic output, and vaccine responses. This transient hepatic reconstitution approach enhanced antitumor immunity and improved vaccine efficacy without triggering autoimmune reactions, offering a promising new strategy for combating immune aging and its associated vulnerabilities to infection, cancer, and vaccine failure.
As we age, our immune systems undergo profound changes that leave us more vulnerable to infections, less responsive to vaccines, and at higher risk for cancer. This age-related immune decline, known as immunosenescence, represents one of the most significant challenges in modern medicine. Now, a groundbreaking study published in Nature reveals a novel approach to reversing this decline using mRNA technology delivered to the liver.

The research, led by scientists from the Broad Institute of MIT and Harvard, demonstrates how transiently repurposing the liver as a "factory" for immune-stimulating factors can restore youthful immune function in aged mice. This innovative approach combines mRNA technology with precise immune modulation to address multiple aspects of immune aging simultaneously.
The Problem of Immune Aging
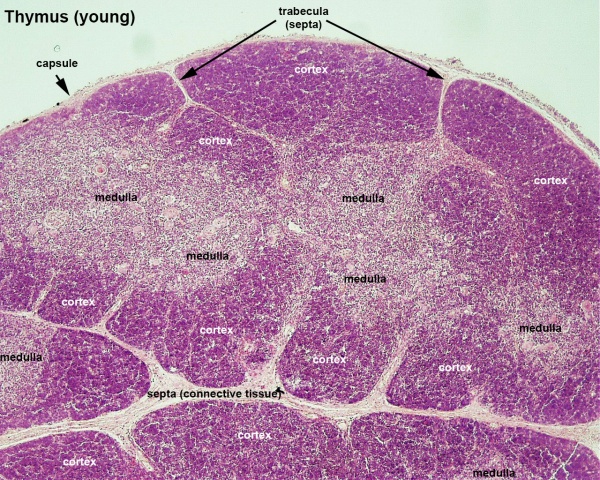
Immune aging affects nearly every aspect of our body's defense system. The thymus, the organ responsible for producing new T cells, undergoes involution—shrinking and losing function—as we age. This leads to reduced output of naive T cells, decreased T cell receptor diversity, and impaired responses to new pathogens and vaccines. Additionally, existing T cells accumulate dysfunctional states, creating a perfect storm of immune vulnerability.
Previous attempts to rejuvenate immune function have faced significant limitations. Hormone therapies, cytokine treatments, and other interventions have shown only modest results and often come with toxicity concerns or lack clinical feasibility. The new study, published in Nature, takes a fundamentally different approach by targeting the liver as a temporary production site for immune-restorative factors.
The Three-Factor Solution
Through comprehensive multi-omic analysis of young and aged mice, researchers identified three key signaling pathways that decline with age: Notch signaling, Fms-like tyrosine kinase 3 ligand (FLT3L) signaling, and interleukin-7 (IL-7) signaling. These pathways are crucial for T cell development, survival, and function.

The team developed mRNA constructs encoding Delta-like ligand 1 (DLL1, which activates Notch), FLT3L, and IL-7. These mRNAs were packaged into SM-102 lipid nanoparticles (LNPs) similar to those used in COVID-19 vaccines and delivered to the liver through intravenous injection. The liver was chosen as the target organ because of its unique hemodynamics, preserved protein-synthesis capacity even in advanced age, and ability to support adaptive immunity.
How the Therapy Works
When delivered to hepatocytes, the mRNAs produce the three immune factors that then enter circulation. DLL1 is expressed on hepatocyte surfaces, while FLT3L and IL-7 are secreted into the bloodstream. This creates a temporary, rejuvenated immune environment that mimics the supportive conditions found in younger individuals.
The mRNA approach offers significant advantages over traditional recombinant protein therapies. Recombinant cytokines clear rapidly from the body, requiring frequent high-dose administrations that often cause significant toxicity. In contrast, mRNA allows for more controlled, transient protein production with reduced side effects. The study found that mRNA-encoded factors achieved sustained levels with lower peak concentrations than recombinant proteins, minimizing inflammatory responses.
Restoring Youthful Immune Function
The results were striking. In aged mice (72 weeks old), treatment with the three-factor mRNA combination (DFI) for 28 days produced multiple beneficial effects:
- Increased naive T cells: Both frequency and absolute numbers of circulating naive CD4+ and CD8+ T cells rose significantly
- Enhanced thymic output: The therapy boosted de novo thymopoiesis without affecting hematopoietic stem cell composition
- Improved dendritic cell function: Conventional type 1 dendritic cells, critical for antigen presentation, expanded and showed enhanced co-stimulatory capacity
- Balanced B cell populations: The treatment reduced age-associated B cells while expanding mature follicular-like B cells
Perhaps most importantly, the therapy worked by amplifying committed lymphoid progenitors and facilitating their recruitment to the thymus, rather than reprogramming hematopoietic stem cells. This more targeted approach reduces the risk of unintended consequences while effectively addressing the specific deficits of immune aging.
Practical Benefits: Vaccines and Cancer
The researchers tested whether these immunological improvements translated into practical benefits. In vaccination experiments, aged mice preconditioned with DFI showed dramatically improved responses to ovalbumin vaccines. They generated approximately twice as many antigen-specific CD8+ T cells as control mice and produced higher levels of protective cytokines like IL-2 and IFNγ upon antigen recall.
Even more impressive were the results in cancer models. In both melanoma and colon carcinoma models, DFI treatment improved antitumor immunity in aged mice. When combined with immune checkpoint inhibition (anti-PDL1 therapy), DFI drove complete tumor rejection in 40% of aged mice with aggressive melanoma—a remarkable result given that all control mice succumbed to the cancer despite receiving the same checkpoint therapy.
Mechanism of Antitumor Action
Analysis of tumor-infiltrating lymphocytes revealed that DFI treatment increased the frequency of intratumoral CD8+ T cells and enriched for tumor-specific T cells. These cells showed lower expression of exhaustion-associated genes and greater clonal diversity, indicating broader recruitment and more effective tumor recognition. The therapy essentially created a more youthful, responsive T cell repertoire within the tumor microenvironment.
Safety and Reversibility
One of the most critical aspects of any immune-modulating therapy is safety. The researchers conducted extensive safety assessments across multiple models:
- Autoimmunity models: In NOD mice prone to type 1 diabetes, DFI did not accelerate disease onset or increase frequencies of autoreactive T cells
- Tolerance models: In mice with intact central tolerance to ovalbumin, DFI did not break tolerance or induce autoantibodies
- Experimental autoimmune encephalitis: DFI did not worsen disease in this model of central nervous system autoimmunity
The effects of DFI were also reversible. When treatment stopped, thymic output returned to baseline within weeks, and immunological benefits waned. This reversibility represents a safety feature, allowing clinicians to control the duration and intensity of immune modulation.

Broader Implications
This research represents more than just a potential therapy for immune aging—it demonstrates a new paradigm for using the liver as a transient production site for therapeutic proteins. The liver's unique characteristics make it an ideal platform for systemic delivery of factors that decline with age or disease.
The study's senior author, Feng Zhang, noted in the Nature publication that "these findings underscore the promise of mRNA-based strategies for systemic immune modulation and highlight the potential of interventions aimed at preserving immune resilience in ageing populations."
Future Directions
While the results are promising, several questions remain for translation to humans. The long-term consequences of repeated administrations need further study, as do potential age-related differences in liver function and mRNA processing. Additionally, researchers may explore whether similar approaches could address other aspects of immune aging beyond T cell function, such as myeloid dysfunction or stromal network alterations.
The transient nature of mRNA delivery means that sustained benefits would require repeated administrations. Future work may focus on optimizing dosing schedules or developing longer-lasting formulations while maintaining the safety profile demonstrated in this study.
Conclusion
The ability to rejuvenate aged immune systems represents a major advance in our fight against age-related diseases. By combining mRNA technology with precise immune modulation, researchers have developed a strategy that addresses multiple aspects of immune aging simultaneously while maintaining safety and reversibility.
As our population ages and faces increasing challenges from infections, cancer, and vaccine-resistant pathogens, approaches like hepatic reconstitution of immune factors offer hope for maintaining immune resilience throughout life. This research not only provides a potential therapy for immune aging but also establishes a new framework for using mRNA and the liver to restore declining physiological functions—a concept that could extend far beyond immunology to address numerous age-related conditions.





