Young Immune Cells Reverse Brain Aging and Alzheimer's Symptoms in Groundbreaking Study
Cedars-Sinai researchers have made a significant breakthrough in neurodegenerative disease research by creating 'young' immune cells from human stem cells that successfully reversed cognitive decline and Alzheimer's symptoms in mice. The lab-grown mononuclear phagocytes improved memory performance and preserved brain structure in aging and Alzheimer's-affected mice, suggesting a potential new pathway for personalized anti-aging therapies. This innovative approach could lead to regenerative treatments that address age-related cognitive decline through indirect brain protection mechanisms.
In a groundbreaking development that could reshape our approach to neurodegenerative diseases, researchers at Cedars-Sinai Medical Center have successfully reversed brain aging and Alzheimer's symptoms using lab-grown immune cells derived from human stem cells. This innovative research, published in Advanced Science, demonstrates how 'young' mononuclear phagocytes created from human induced pluripotent stem cells can significantly improve cognitive function and brain health in aging mice and mouse models of Alzheimer's disease.
The Science Behind the Breakthrough
The research team, led by Dr. Clive Svendsen, executive director of the Board of Governors Regenerative Medicine Institute, took a novel approach to addressing age-related cognitive decline. Previous studies had shown that transfusions of blood or plasma from young mice could improve cognitive function in older mice, but translating this into practical human therapies proved challenging. The Cedars-Sinai team's solution was to create young immune cells that could be manufactured in the laboratory, providing a more scalable and controllable therapeutic approach.
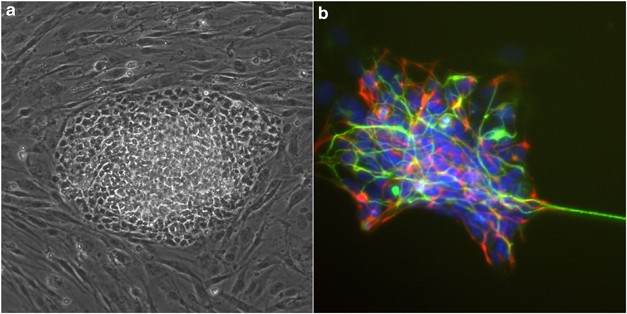
These specialized immune cells, known as mononuclear phagocytes, naturally circulate throughout the body to clear harmful substances. However, their effectiveness diminishes significantly with age. By using human induced pluripotent stem cells—adult cells reprogrammed to an early embryonic-like state—researchers were able to generate new, young mononuclear phagocytes with restored functionality.
Remarkable Results in Animal Models
When these laboratory-grown young immune cells were infused into aging mice and mouse models of Alzheimer's disease, the results were striking. The treated animals demonstrated significantly improved performance on memory tests compared to untreated control groups. More importantly, researchers observed substantial improvements in brain structure and cellular health.
The brains of treated mice contained higher numbers of 'mossy cells' within the hippocampus, a brain region crucial for learning and memory formation. As Dr. Alexandra Moser, lead author of the study, explained, "The numbers of mossy cells decline with aging and Alzheimer's disease. We did not see that decline in mice receiving young mononuclear phagocytes, and we believe this may be responsible for some of the memory improvements that we observed."
Preserved Brain Immune Function
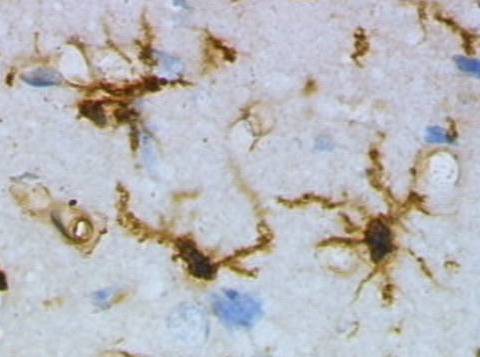
Beyond the improvements in memory and mossy cell preservation, the research revealed another crucial benefit: healthier microglia. These specialized immune cells within the brain are responsible for detecting and clearing damaged tissue. In normal aging and Alzheimer's disease, microglia lose their long, thin branches, impairing their function. However, in mice treated with young mononuclear phagocytes, these branches remained extended and active, suggesting preserved immune and cognitive function.
Indirect Protection Mechanism
One of the most intriguing aspects of this research is how these young immune cells exert their beneficial effects. Since the mononuclear phagocytes did not appear to cross into the brain, researchers believe they may influence brain health indirectly through mechanisms in the bloodstream. The team proposes several possibilities: the cells could release anti-aging proteins or tiny extracellular vesicles capable of entering the brain, or they might remove pro-aging factors from the blood, thereby protecting the brain from harmful effects.
Future Implications and Personalized Medicine
This breakthrough holds significant promise for developing new treatments for age-related cognitive decline and neurodegenerative diseases. As Dr. Jeffrey A. Golden, executive vice dean for Education and Research, noted, "Because these young immune cells are created from stem cells, they could be used as personalized therapy with unlimited availability. These findings show that short-term treatment improved cognition and brain health, making them a promising candidate to address age- and Alzheimer's disease-related cognitive decline."
The research represents a significant step toward regenerative, stem-cell-based anti-aging therapies that could potentially be tailored to individual patients. While much work remains to translate these findings into human treatments, the study provides a compelling new direction for addressing one of healthcare's most challenging problems: age-related cognitive decline and neurodegenerative diseases.